The New England Journal of Medicine carries in its latest issue (June 28, 2007), an article on the ruling in Abney et. al v. Amgen, Inc. by the Sixth Circuit in March 2006. The ruling, while not particularly controversial, has incited a debate on the responsibilities of pharmaceutical companies sponsoring trials and partaking academic medical centers towards subjects who participate in them.
The case itself is straightforward. The plaintiffs were all Kentucky residents suffering from Parkinson’s disease enrolled in a phase II randomized, double-blind, placebo controlled trial of a synthetic protein called glial cell-line derived neurotropic factor (GDNF) at the University of Kentucky Medical Center in 2003. Amgen, which sponsored this trial, had been trying to develop a safe and effective method of administration of this protein since 1994 and had, a priori, accumulated some supportive data from an open-label study (a kind of study where no control group exists and patients, unlike in a blind study, are aware that they are taking the drug). Amgen, as is customary, executed a clinical-trial agreement with the university to set up the trial and submitted the study protocol to the University’s institutional review board (IRB). Further, as stated in the piece:
“The protocol and consent form stated that at the end of the trial, the subjects “may elect to continue treatment for up to an additional 24 months.” The consent form also stated that subjects could be withdrawn from the study if the investigators deemed that the risk to them outweighed the benefits, if they were noncompliant with instructions, or “if the agency funding the study decides to stop the study early for a variety of reasons.”
The trial showed disappointing results based on analysis of the primary efficacy end point (percent change in the baseline motor score at 6 months). Though the improvement among those receiving GDNF was slightly greater than among those receiving placebo, the difference did not achieve statistical significance. Nevertheless, Amgen decided to continue the trial, with all 34 subjects receiving open-label GDNF. However, in September 2004, Amgen informed the university that it had decided to stop the trial, citing three concerns. First, neutralizing antibodies that could also attack naturally occurring GDNF had developed in several subjects. Second, brain lesions had been discovered in studies of GDNF in primates. Third, the drug apparently lacked efficacy. Before making its announcement, Amgen consulted with Food and Drug Administration (FDA) officials, who agreed that termination of the study would be reasonable but said the decision was entirely Amgen’s.
Many subjects, however, believed that their conditions had improved and wanted to continue receiving GDNF. Amgen met with FDA officials to discuss whether “compassionate use” of GDNF would be appropriate. The FDA granted its permission but gave Amgen discretion to decide whether it would provide the drug.”
The company, after seeking advice of eight outside experts seven of whom had advised it before (to terminate the use of the drug), declined, and the subjects sued, alleging that the termination decision was financially motivated, an allegation that Amgen vehemently disputed. The plaintiffs also questioned the pertinence of the findings of the primates’ study and challenged the view that the antibodies were harmful.
The plaintiffs advanced three legal theories to support their motion for a preliminary injunction. First, they claimed that GDNF is beneficial to them and claimed that Amgen is contractually obligated to supply them with GDNF; second, that Amgen was liable under a theory of promissory estoppel (this legal doctrine proposes that if Person A reneges on a promise on which Person B has reasonably relied, to B’s detriment, fairness may require that A make B whole, even if the promise was not set forth in a valid contract) and thirdly, that Amgen owed them a fiduciary duty that was breached by unreasonably denying them GDNF.
The federal district court, relying on an opinion in a similar case, Suthers v. Amgen from the Southern District of New York, denied all the claims. On the first, it said that no contract was breached since none existed between the plaintiffs and Amgen; even if one had existed, the Informed Consent Document allowing Amgen to terminate the study for scientific reasons (a usual practice followed in such trials)ensured that Amgen would still have no duty towards the plaintiffs. Also, the trial being conducted at the university by doctors who were under its employment, the principal investigators were not Amgen agents and therefore, the principal/agent rule could not apply. On the second claim, promissory estoppel required a promise (to continue to provide GDNF following termination of the study) that did not exist. As for the third claim, the court indicated that Amgen had reasons other than the benefit of the plaintiffs for sponsoring the study, circumstances that would indicate that “the parties agreed that one party would act in the interest of the other” did not exist. Hence, it could not be held that Amgen owed a fiduciary duty to the plaintiffs. The appeals court, while affirming this decision, ultimately suggested that the plaintiffs might have a case against the university’s institutional review board and the physician investigators involved in the trial.
This case raises several questions. First of all, clinical trial agreements between industry and academic institutions are usually not revealed to subjects while recruiting them for a study. Also, the investigators themselves not being fully conversant with its details, may misrepresent its meaning and implications. Should institutions appoint an authority conversant with the specifics to deal exclusively with such matters? Secondly, in conducting a trial, the goal of the company is primarily scientific, not therapeutic; monetary or other business considerations might compel termination of the trial before its therapeutic value is fully realized for subjects enrolled in it. If ethical considerations in such instances mandate the continuation of the treatment past the termination of the trial, should the obligation be made enforceable through appropriate contract language (the article suggests so but should the company be made to bear the entire expense at that point or the burden shifted upon the subjects themselves)? Thirdly, should the determination of efficacy also make allowance for the patients’ own subjective opinions?
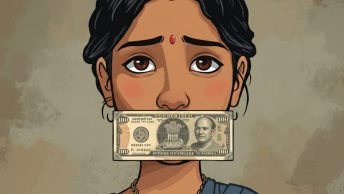
In India, the ICMR guidelines issued in 2000 mentions, in the obligations of investigators to prospective subjects, that they must explain the ‘benefits that might be reasonably expected as an outcome of research to the subject or to others’ and that the ‘investigator should not give any unjustifiable assurances to prospective subjects, which may influence the subject’s decision to participate in the study’ – these are helpful but general statements that do not clarify the post-trial obligations or the delineation of obligations between the industry sponsor and the academic investigator. It might be worthwhile to define this separately in some detail. Also, ethics committees of host institutes are given the responsibility of oversight of any trial. How frequently these bodies meet and how effectively they function ought to be examined.






Dear Mr.Dilip,
Thanks for the inaugural post. But I would appreciate if you place more emphasis, than what you have done, on that part of the post which has direct relevance to Indian health policy. The part which has relevance to India appears remote, and is buried in the post. It ought to have come out prominently in the post to sustain our interest, many of us being India-centric!
I have just emailed you an edit in Business-standard on a new Bill on health care policy. I would appreciate if you could share your insight on this Bill.
Dear Venkat,
Thanks for your pointed suggestion. I will attempt to word my future articles differently next time keeping in mind a more ‘india-centric’ approach. As a related matter, I wrestled initially with the question of relevance of this topic to India but eventually decided to write on it for a couple of reasons: (1) the organization and conduct of clinical trials is largely along similar lines in India; whereas the legal specifics of this case itself were not very pertinent to the Indian context, the questions raised therein appear to have broader implications that are equally relevant especially given that such trials are expected to grow in the coming years (2) this week’s news item (http://www.hindu.com/thehindu/holnus/002200706270342.htm) that the government was planning to regulate clinical trials which made me wonder whether this was an aspect of clinical trials that merits attention.
Thank you for sending that link from the Business Standard. I found more details of the same item in other newspapers and from what I gather so far, this is my understanding: all clinical establishments will have to be registered, minimum standards prescribed for each category will have to be met by the end of a grace period, the prescription of standards and review of compliance being done by a National Council of Standards to be headed by the DGHS and comprising of medical/dental/nursing/pharmacy representatives. So far it is unexceptionable but the devil is often in the details – to assess the effectiveness and implications, it would be helpful to have a look at the actual provisions of the bill which I have not yet been able to find on the web.